Abstract
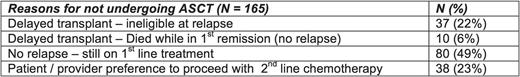
Background: High dose chemotherapy followed by ASCT is an effective strategy for patients with MM and remains standard first line treatment for all eligible MM patients. However, randomized clinical trials show equivalent outcomes when ASCT is delayed until first relapse. Some patients who have PBSCs collected for a delayed ASCT never proceed to an ASCT despite experiencing disease relapse after 1st line therapy. The impact of this non-utilization of collected PBSCs for ASCT on the survival outcomes in MM is not clear. Thus, we carried out a retrospective analysis to evaluate the reasons for non-utilization of collected PBSC for ASCT and its outcomes.Method: The Mayo Clinic EMR was queried for all patients who underwent collection of PBSCs for ASCT consideration. From June 2003 to June 2014 we identified 1,434 patients who underwent ASCT. 194 collected PBSCs but never proceeded to an ASCT. We excluded the following: 16 MM patients lost to follow up, 3 MM patients as they underwent allogenic stem cell transplant, 6 MM patients who underwent ASCT at outside institutions, 2 patients with systemic AL amyloidosis and 2 patients with Waldenstroms Macroglobulinemia. Clinical and outcomes data were abstracted retrospectively on the remainder of the 165 MM patients. Results: Of the 165 patients included in the final analysis, the median age was 63 years (range: 32 - 73) and 57% were male. The median time from diagnosis to apheresis was 6.4 months (2.3 - 12.5) for this cohort with a median follow-up of 49.6 months (5 - 131). Reasons why ASCT eligible patients who collected PBSCs never underwent ASCT are listed in Table 1. The most common reason for not undergoing an ASCT was not experiencing a disease relapse while still on 1st line treatment. There were 75 (45%) patients in this cohort who experienced an initial disease relapse but did not undergo a delayed ASCT due to either a) ineligibility at 1st disease relapse (N = 37, 22%) or b) patient/provider preference (N = 38, 23%). The median OS since diagnosis for these 75 patients who did not proceed with a delayed ASCT upon initial disease relapse was 118 months (95% CI: 35 - 118).Conclusions: In the real world, when a "delayed transplant" strategy is chosen, a significant number of patients (~22%) are ineligible to receive ASCT at relapse. This is a first of its kind analysis describing the reasons for non-utilization of harvested PBSC for ASCT. Our study provides an important tool for patients and care providers in making an informed decision while deciding between early vs. delayed ASCT.
Gertz: Celgene, Novartis, Smith-Kline, Prothena, Ionis, Amgen: Honoraria; Millennium: Consultancy, Honoraria. Dingli: Alexion Pharmaceuticals: Consultancy; Karyopharm Therapeutics: Research Funding; Janssen: Consultancy; Takeda: Consultancy; Millenium: Consultancy. Dispenzieri: Celgene, Millenium, Pfizer, Janssen: Research Funding. Kapoor: Takeda, Celgene and Amgen: Research Funding. Kumar: Celgene, Millennium/Takeda, Onyx, AbbVie, Janssen, Sanofi, Novartis, Amgen, Genentech, Merck, Oncopeptides, Roche, Skyline Diagnostics: Research Funding; Skyline: Honoraria; Celgene, Millennium, BMS, Onyx, Janssen, Noxxon, AbbVie, Amgen, Merck, Oncopeptides, Skyline Diagnostics, Takeda: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal